ORIGINAL ARTICLE |
||
Year : 2021 | Volume : 3 | Issue : 2| Page : 12-19 |
||
![]()
Comparitive Comparative evaluation of dexmedetomidine and fentanyl with ropivacaince for epidural analgesia in lower limb orthopedic surgeries
HimalyYogendra Vinayak1*, SB Gangadhar2
1*Postgraduate Student, 2 Professor and Head, Department of Anaesthesia, Sri Siddhartha Medical College, SSAHE, Tumkur Karnataka India
* Address for Correspondence:
Dr. HimalyYogendraVinayak, Post graduate Student, Dept of Anaesthesia, Sri Siddhartha Medical College, SSAHE Tumkur Karnataka India. Email:
Abstract
Background: Epidural analgesia is of great importance in surgical field for postoperative analgesia. Epidural analgesia is a very good technique for post operative analgesia. It is quicker acting and more efficient than any other analgesic technique.Most commonly used local anaesthetics are Ropivacaine and Bupivacaine. Material and method: Eighty two patients were selected under American Society of Anaesthesiologist grade 1 and 2 . All the patients were divided into two groups of forty one each. Group RD receivedRopivacaine 15 ml of 0.75 % withDexmeditomidine and Group RF recievedRopivacaine with Fentanyl 1 mcg /kg epiduraly. Haemodynamic parameters like oxygen saturation, heart rate, time of onset of analgesia upto dermatome level T10 and duration of analgesia, motor blockade and parameters of sedation scores were observed and compared . At the end of the study all the data were analyzed using independent sample t test, ANOVA test, Chi square test. Results: The onset of analgesia at T10 dermatomal level was significantly earlier in the RD group (6.68±0.47) as compared to the RF group (9.52±0.58) P<0.05. Conclusion: When given epiduraly as a post operative analgesia, dexmeditomidine as an adjuvant provide stable cardio respiratory parameters, duration of analgesia is long lasting, number of rescue analgesia required was less or nil in comparison to fentanyl used as an adjuvant to ropivacaine in epidural analgesia postoperatively.
Key words: Dexmedetomidine, epidural anesthesia, fentanyl, lower limb surgery, ropivacaine
Introduction
Epidural Analgesia provides long term potent analgesia with relatively less haemodynamic side effects. And Epidural analgesia is used for postoperative pain relief, for long term surgeries or surgeries of unpredictable duration.
Serious complication of epidural analgesia are hypotension, nausea,vomiting, bronchoconstriction etc. Special care needs to be taken in terms of epidural haematoma, epidural abscesses.[1] Epidural analgesia is most preferred by surgeons as it will allow early mobilizationand painless recovery.
Ropivacaine and bupivaciane are the most commonly used local anaesthetics used.
Ropivacaine is a long acting amide group local anaesthetic agent. Mechanism of action of ropivacaine is that it blocks nerve signal by inhibiting the sodium influx in the nerve fibers. Ropivacaine is more efficient than Bupivacaine as it less lipophillic and hence does not penetrate large myelinated nerve fibers and will produce less motor block. Ropivacaine provides better sensory blockade which makes it appropriate analgesic agent.
Bupivacaine's most common side effect is cardio toxicity, this cardiotoxicity is due to S enantiomer. Cardio-toxicity manifest as hypotension and bradycardia. Ropivacaine lacks these side effect of cardiotoxicity.
Fentanyl is an opioid and narcotic medication. Fentanyl is commonly used as a pain medication. Fentanyl is used in the form of injection, skin patch, nasal spray. Fentanyl is an opioid which has potent adjuvant effect of analgesia. Fentanyl acts on opioid receptor. It is around 100 times more stronger than morphine. Fentanyl has high lipid solubility and hence penetration in the central nervous system is easier. It produces good supraspinal analgesia. Side effect of fentanyl are nausea, vomiting, dry mouth, constipation, respiratory depression, bradycardia, fatigue, anorexia, dyspepsia and pruritis. Major side effect of fentanyl are physical dependence, muscle rigidity.[2, 3]
Dexmeditomdine is an alpha 2 adrenoreceptor agonist. Mechanism of action of dexmeditomidine is by blocking presynaptic alpha 2 adrenoreceptor it inhibits the release of norepinephrine. Dexmeditomidine causes decrease in sympathetic tone. Sympathetic, neuroendocrine and haemodynamic parameters are decreased. Main site of action of fentanyl is the locus cerulus of the brain.
Uses of dexmeditomidine are - it can be used as a sedative and analgesic agent in intensive care for intubated patients on Ventilator. It can be used an analgesic in pain management. Desirable effect of dexmeditomidine for intraoperative and intensive care patients is that it reduces delirium, agitation. Dexmeditomidine provides analgesia and sedation with cardio stable effect without causing respiratory depression. We used dexmeditomidine with ropivacaince and fenatanyl with ropivacaine as an adjunct to compare their efficacy.
Materials and methods
A prospective randomized double blinded study was conducted at Sri Siddhartha Medical College, Tumakuru, in Anaesthesiology Department between 2019-2021 after approval of research ethics committee.
Eighty two patients between age group of 18-60 years, both sex, who underwent lower limb orthopaedics surgery with the physical status, American Society of Anesthesiologist (ASA) 1 and 2 were included after taking an informed consent. Patients showing hypersensitivity to any of study drugs, patients with comorbities like daibetes mellitus, cardiac disease, hypertension, chronic obstructive disease, respiratory depression, coagulation abnormalities, spinal deformities, patients taking alpha-2 adrenergic agonists, tricyclic antidepressants, any antipsychotic drugs, antiarrhythmics, beta blockers, anticoagulants and opioids were excluded.
Patients were randomly divided into two groups ropivacaine + dexmeditomidine is group RD and ropivacaine+ fentanyl is group RF.
Premedication given to the patient before the surgery was inj alprazolam 0.25 mg. On arrival to the operation theatre, patient was identified and under aseptic precautions 18 gauge intravenous line was established. Baseline parameters including heart rate, saturation , blood pressure, electro cardiography were noted. Patient was in sitting position and under aseptic precaution 25 gauge spinal needle was introduced at lumbar level L3-L4 space. Free backflow of cerebrospinal fluid was noted. 3.8 cc of injection 0.5% bupvacaine heavy was given in the subarchanoid space. Again under aseptic precaution 18 Gauge B Braun Touhy needle was introduced at Lumbar level L2-L3 space. Epidural space was confirmed with loss of resistance and hanging drop technique. Epidural catheter was secured.[4, 5]
After an uneventful surgical procedure patient was shifted to the post operative ward. On complaint of postoperative pain depending on the group rescue analgesia was given. Group RD received 15 ml of inj 0.2% ropivacaine intravenouslyand inj 1µg/kg of dexmeditomitine(n=42) intravenously. Group RF received 15 ml of Inj 0.2% ropivacaine intravenously and inj 1µg/kg of fentanyl(n=42) intravenously. Baseline parameters including heart rate, saturation , blood pressure, echo cardiography were noted. Time period and quality of analgesia, number of rescue analgesia and complication and side effects were noted. Mean and Standard Deviation was used to express the data. At the end of study all the data was compiled and subjective analysis using independent sample t test, ANOVA test, Chi square test was done.[6,7]
Results
A total of Eighty two patients who underwent lower limb surgery were enrolled for the study and were randomly divided into two groups. The demographic characteristics in both the groups exhibited marked similarities and did not show any statistical significant difference.
Table 1 and Figure 1 shows the comparison of the onset of sensory and motor blockade. The onset of analgesia at T10 dermatomal level was significantly earlier in the RD group (6.68±0.47) as compared to the RF group (9.52±0.58) P<0.05. The other early block characteristics also exhibited similar results as dexmedetomidine not only provided a higher dermatomal spread but also helped in achieving the maximum sensory anaesthetic level in a shorter period as compared to Fentanyl. Motor block was assessed using modified Bromage scale and complete motor block was achieved significantly earlier in the (12.46±2.31) patients who were administered dexmedetomidine as compared to RF group (23.41±4.98) respectively P<0.05.[8,9]
Table 1: Comparison of Onset of sensory blockade, Onset of motor blockade and time for complete block
Parameters |
Group RD |
Group RF |
P-value¶ |
Onset of sensory blockade |
6.68±0.47 |
9.52±0.58 |
0.012 |
Onset of motor blockade |
12.46±2.31 |
15.58±3.93 |
<0.001 |
Time for complete block |
17.19±3.12 |
23.41±4.98 |
<0.001 |
¶Independent sample t-test
Figure 1: Comparison of Onset of sensory blockade, Onset of motor blockade and time for complete block

Table 2:Physical characteristics of study groups and duration of surgery
Parameters |
Group RD (N=40) |
Group Rf(N=40) |
t-value |
P-value¶ |
Age |
38.9±12.6 |
43.9±14.5 |
-1.671 |
0.099 |
Weight |
71.3±10.9 |
70.4±10.8 |
0.350 |
0.727 |
BMI |
23.2±2.9 |
22.3±3.3 |
1.284 |
0.203 |
Duration of Surgery (in minutes) |
99.3±6.3 |
101.1±6.5 |
-1.227 |
0.321 |
¶Independent sample t-test
Figure 2: Physical characteristics of study groups and duration of surgery
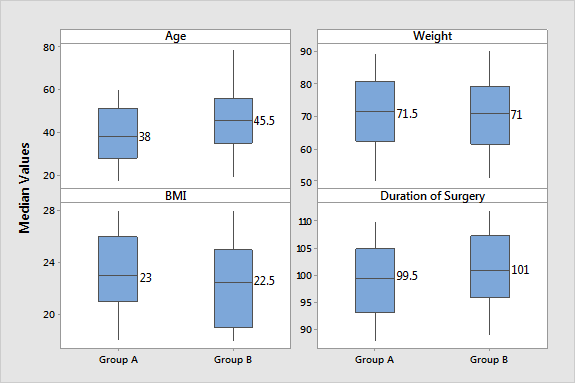
Table 2 shows the physical characteristics of study group and duration of surgery .There was no statistically significant difference in mean age, weight, BMI and duration of surgery found between the groups P>0.05 indicating the subject in both groups are very well matched.
Table 3, 4, 5, 6 shows comparison of saturation, heart rate, systolic blood pressure, diasystolicblood pressure, mean arterial pressure. (4%) patient in Group RF and (20%) patients in Group RD developed bradycardia, which were treated with injection atropine 0.6 mg. The increase in pulse rate at 90 min might be due to sudden arousal of the patient, but it remained below the baseline. Moreover, the difference was nonsignificant (P > 0.05) at all varied time intervals, showing the hemodynamic stability of the adjuvant, dexmedetomidine. (Figure 3, 4, 5 and 6)
Table 3 shows the comparison of oxygen saturation SPO2 levels of the two groups .There was no change of SPO2 levels observed between the groups at all time points P>0.05.(10)
Table 3: Comparison of SPO2
SPO2 |
Group RD (N=40) |
Group RF (N=40) |
t-value |
P-value¶ |
0min |
98.8±0.5 |
98.6±0.7 |
1.549 |
0.125 |
15min |
98.7±0.6 |
98.8±0.5 |
-0.866 |
0.389 |
30min |
98.6±0.6 |
98.9±0.4 |
-1.342 |
0.184 |
45min |
98.7±0.6 |
98.9±0.4 |
-1.342 |
0.184 |
1hr |
98.7±0.6 |
98.8±0.4 |
-1.342 |
0.184 |
2hrs |
98.8±0.6 |
98.7±0.4 |
-0.192 |
0.848 |
3hrs |
98.7±0.6 |
98.9±0.4 |
0.200 |
0.842 |
4hrs |
98.7±0.6 |
98.8±0.4 |
-0.192 |
0.848 |
6hrs |
98.9±0.6 |
98.7±0.4 |
0.200 |
0.842 |
F-value |
0.361 |
1.326 |
|
|
P-value€ |
0.981 |
0.25 |
||
¶ Independent sample t-test, € Repeated measure ANOVA
Figure 3: Comparison of SPO2

Table 4: Comparison of Heart Rate
Heart Rate |
Group RD (N=40) |
Group RF (N=40) |
t-value |
P-value¶ |
0min |
99.9±8.6 |
98.0±10.0 |
-1.044 |
0.300 |
15min |
98.8±10.7 |
95.8±15.3 |
-0.571 |
0.569 |
30min |
94.1±17.6 |
95.2±14.4 |
0.935 |
0.352 |
45min |
92.6±12.7 |
95.6±13.0 |
1.183 |
0.241 |
1hr |
91.6±12.2 |
92.5±12.5 |
1.410 |
0.163 |
2hrs |
89.8±11.6 |
95.6±13.0 |
0.064 |
0.949 |
3hrs |
87.8±11.8 |
95.2±14.4 |
-0.335 |
0.738 |
4hrs |
91.8±16.5 |
91.7±13.2 |
-1.597 |
0.114 |
6hrs |
87.8±11.8 |
92.5±12.5 |
-0.292 |
0.771 |
F-value |
9.636 |
24.824 |
|
|
P-value€ |
<0.001 |
<0.001 |
||
¶ Independent sample t-test, € Repeated measure ANOVA
There was no statistical difference in mean heart rate between groups observed at all time points, however repeated measure ANOVA showed significant decline in heart rate over the period of time P<0.05.
Figure 5: Comparison of Heart Rate

It is observed that, Systolic blood pressure, Diastolic blood pressure and Mean blood pressure increased significantly from 0 minutes to about 1 hour and it declines back to the normal at later stage of time P<0.05.
Table 5: Comparison of Systolic Blood Pressure
Systolic Blood Pressure |
Group Rd(N=40) |
Group RF (N=40) |
t-value |
P-value¶ |
0min |
121.6±9.8 |
122.7±9.8 |
-0.502 |
0.617 |
15min |
124.7±10.4 |
123.3±9.5 |
0.628 |
0.532 |
30min |
133.6±16.6 |
131.2±14.4 |
0.704 |
0.483 |
45min |
134.3±15.7 |
129.6±9.2 |
1.644 |
0.104 |
1hr |
134.3±15.7 |
129.6±9.2 |
1.644 |
0.104 |
2hrs |
131.3±14.1 |
132.7±13.7 |
-0.450 |
0.654 |
3hrs |
130.8±11.7 |
128.7±27.3 |
4.878 |
0.000 |
4hrs |
124.9±14.9 |
123.1±19.7 |
-1.561 |
0.141 |
6hrs |
122.8±13.7 |
122.0±20.3 |
-0.238 |
0.752 |
F-value |
5.972 |
16.586 |
|
|
P-value€ |
<0.001 |
<0.001 |
||
¶ Independent sample t-test, € Repeated measure ANOVA
Figure 5: Comparison of Systolic Blood Pressure

Table 6: Comparison of Diastolic Blood Pressure
Diastolic Blood Pressure |
Group RD (N=40) |
Group Rf (N=40) |
t-value |
P-value¶ |
0min |
89.1±8.8 |
88.9±9.2 |
-0.397 |
0.693 |
15min |
91.4±13.6 |
92.9±10.5 |
0.056 |
0.956 |
30min |
92.8±9.7 |
92.7±10.6 |
0.660 |
0.511 |
45min |
96.0±7.9 |
96.6±7.9 |
0.845 |
0.670 |
1hr |
97.0±10.5 |
94.9±12.1 |
-0.820 |
0.703 |
2hrs |
96.2±7.9 |
95.1±10.8 |
-0.196 |
0.231 |
3hrs |
96.0±8.1 |
94.3±9.8 |
2.825 |
0.006 |
4hrs |
90.8±13.6 |
91.4±11.6 |
0.820 |
0.415 |
6hrs |
89.7±10.5 |
88.8±9.9 |
0.393 |
0.696 |
F-value |
8.591 |
18.394 |
|
|
P-value€ |
<0.001 |
<0.001 |
||
¶ Independent sample t-test, € Repeated measure ANOVA
Figure 6: Comparison of Diastolic Blood Pressure

Discussion
In our study we have evaluated and compared efficacy of dexmedetomidine versus fentanyl as an adjuvant to ropivacaince in lower limb epidural analgesia. As such in our study no significant difference was seen in the time taken for the onset of complete motor block between dexmetomidine and fentanyl group , however we did notice that dexmeditomidine group achieved the motor and sensory block faster than fentanyl group. Similar findings were found in by study of Mahendru et al. [11, 12] The reason behind this can be highly alpha 2 adrenergic selective receptor agonist dexmeditomodine. Dexmeditomidine as causes analgesia by blocking of the c fibers. Alpha 2 agonism leads to decrease in transmission of nociceptive signals like substance p.
Many previous studies have reported that need for rescue analgesics is comparatively nil in dexmeditomidine group. In one study conducted by bajwa et al it was proven that Duration of the time taken for onset of sensory block was earlier for dexmeditomidine than in fentanyl group. Dexmeditomidine provided better and long lasting analgesia when used as an adjuvant to ropivacaine. In our study I have compared the onset of sensory block, motor block in the two groups. In our study we found that Mean onset of sensory block was earlier in group of dexmeditomidine and ropivacaine when compared to fentanyl and ropivacine.[12]
In one study by Kumar Sundar et al, they found that dexmeditomidine was significantly better adjuvant than fentanyl. They found that onset was faster, prolonged. intensity of analgesia. Intensity of analgesia was better than fentanyl, dexmeditomidine was providing sedation scores.
When haemodynamics were compared in two groups systolic blood pressure (SBP), diasystolic blood pressure (DBP), saturation of oxygen(SPO2), heart rate (HR), mean arterial blood pressure (MAP), there was no significant difference in two groups. However one study conducted by Contractor et al showed the probability ofmean arterial pressure and heart rate decrease is higher in dexmedetomidine group when compared with fentanyl group. Similar studies were made by Manoj et al. Manojkumar et al found that when haemodynamics were compared there was heart rate, SBP, DBP, MAP, alpha 2 sympthatetic, norepinephrine release. In our study, there was no significant difference in the haemodynamic of dexmeditomidine and fentanyl as an adjuvant to ropivacaine1. Studies bybajwa et al showed that there was significant fall in heart rate and MAP in Dexmeditomidine group. Bajwa et al showed that no respiratory depression is seen in either groups.[13]
When complications and side effects were compared there was no significant difference seen. Both the group drugs showed less to nil amount of nausea, vomiting, neglible hypotension and bradycadia. In few cases certain amount of respiratory depression was seen in fentanyl group. Known side effect of fentanyl opioid reported is respiratory depression. [14]
Number of rescue analgesia required in my study were relatively less or nil in dexmeditomidine when compared with fentanyl. Our final conclusion is at when given intrathecally as an adjuvant dexmeditomidine is better than fentanyl as it has better haemdynamic stability, prolonged motor as well as sensory block.[13,14]
Conclusion
It was concluded that anesthesia in both the groups was effective and patients were hemodynamically stable. However dexmedetomidine group was better in view of prolonged duration of sensory block, postoperative analgesia with reduced doses of rescue analgesic required and better patient satisfaction score. However, prolonged duration of motor block and sedation produced with Dexmedetomidine may be undesirable for short surgical procedures or ambulatory surgery.
Acknowledgement: Nil
Financial support and sponsorship: Nil
Conflict of interest: Nil
Reference
1. Soni P. Comparative study for better adjuvant with ropivacaine in epidural anaesthesia. Anaesth essays Res, 2016, 10(2): 218-222.
2. SukhminderJit Singh Bajwa, VikramjitArora, JasbirKaur, et al. Comparative evaluation of dexmedetomidine and fentanyl for epidural analgesia in lower limb orthopedic surgeries. Saudi J Anesth Year: 2011 ; 5(4): 365–370.
3. Baglur S, Dinesh K, Ravi M, Somasekheram (2015) A comparative study of epidural ropivacaine 0.75 % alone with ropivacaine plus fentanyl and ropivacaine plus clonidine for lower abdominal and lower limb surgeries, IOSR Journal of Dental and Medical Sciences 14(12): 19-267.
4. Bajwa SJ, Bajwa SK, Kaur J, Singh G, Arora V, Gupta S, et al. Dexmedetomidine and clonidine in epidural anaesthesia: A comparative evaluation. Indian J Anaesth.2011 ;55(2):116-21.
5. Kaur S, Attri JP, Kaur G, Singh TP. Comparative evaluation of ropivacaine versus dexmedetomidine and ropivacaine in epidural anesthesia in lower limb orthopedic surgeries. Saudi J Anaesth. 2014;8:463-9.
6. Jaakola ML, Salonen M, Lehtinen R, Scheinin H. The analgesic action of dexmedetomidine: A novel alpha2-adrenoceptor agonist–in healthy volunteers. Pain.2001 ; 14(1): 13–21.
7. Talke P, Richardson CA, Scheinin M, Fisher DM. Postoperative pharmacokinetics and sympatholytic effects of dexmedetomidine. AnesthAnalg.1997 ; 85(5) : 1136-42.
8. Rastogi B, Gupta K, Rastogi A, Gupta PK, Singhal AB, Singh I. Hemiarthroplasty in high risk elderly patient under epidural anesthesia with 0.75% ropivacaine-fentanyl versus 0.5% bupivacaine-fentanyl: Clinical trial Saudi J Anaesth. 2013;7(2):142-5.
9. Zaric D, Nydahl PA, Philipson L, Samuelsson L, Heierson A, Axelsson K. The effect of continuous lumbar epidural infusion of ropivacaine (0.1%, 0.2%, and 0.3%) bupivacaine on sensory and motor block in volunteers: A double-blind study. RegAnesth. 1996;21:14-25.
10. Lorenzini C, Moreira LB, Ferreira MB. Efficacy of ropivacaine compared with ropivacaine plus sufentanil for postoperative analgesia after major knee surgery. Anaesthesia. 2002;57:424-8.
11. Jaakola ML, Salonen M, Lehtinen R, Scheinin H. The analgesic action of dexmedetomidine: A novel alpha2-adrenoceptor agonist-in healthy volunteers. Pain.Pubmed. 1991;46:281-5.
12. Marja-LeenaJaakola 1, MarkkuSalonen, RistoLehtinen, Harry ScheininComparative evaluation of dexmedetomidine and fentanyl for epidural analgesia in lower limb orthopedic surgeries. Pain. 1991 Sep ; 46(3) : 281-285.
13. K J MC Clellan, D Fluads.Ropivacaine: An update of its use in regional anesthesia.December 2000 60(5):1065-93.
14. Pratibha J S, Rashmi N, Chandrapal B, Kunal T “Dexmedetomidine V/S Fentanyl with 0.75% Ropivacaine for Epidural Anaesthesia in Lower Abdominal Surgeries - A Comparative Study”. J Anest&Inten Care Med. 2017; 3(3) : 555611.
15. Kehlet H. Acute pain control and accelerated postoperative surgical recovery. SurgClin North Am. 1999 ; 79 : 431-43.

Attribution-NonCommercial-ShareAlike
CC BY-NC-SA

An official peer reviewed publication of
Sri Siddhartha Medical College & Research Centre
Constituent College of Sri Siddhartha Academy of Higher Education
(Deemed to be University u/s 3 of UGC Act, 1956)
Accredited 'A' Grade by NAAC
Tumakuru, Karnataka, India. 572107
Research Journal of Medical and Allied Health Sciences is a medium for the advancement of scientific knowledge in all the branches of Medicine and Allied Sciences and publication of scientific research in these fields. The scope of the journal covers basic medical sciences, medicine and allied specialities, surgery and allied specialities, dentistry, nursing, pharmacy, biotechnology, public health and other branches of the allied health sciences. This journal is indexed with Advanced Science Index(ASI), National Science Library and Open J Gate.


E-ISSN : 2582-080X | : editor@ssmctumkur.org , info@ssmctumkur.org

Attribution-NonCommercial-ShareAlike 4.0 International (CC-BY-NC-SA 4.0)